'I had no choice': SJ couple billed more than $2,200 to take ambulance next door

SAN JOSE, Calif. (KGO) -- A San Jose couple says they were billed $2,255 after an emergency room visit led to an unnecessary ambulance ride - approximately 100 yards away.
It was the shortest, yet most expensive ambulance bill Frank Chan and his wife hope to never see again.
"I was shocked," said Chan, staring at the bill in disbelief. "I know exactly how far the distance was."
In November, Chan's wife, Amber drove herself to the emergency department at El Camino Health, an acute care hospital in Mountain View. Amber told the I-Team she was admitted and then transferred to the mental health inpatient clinic - which happened to be the building next door to the ER.
"I wanted to walk, but was told an ambulance was required," Amber said. "I had no choice."
The distance from the ER to the inpatient clinic was approximately 100 yards away.
VIDEO: What you need to know about the cost of visiting the ER

A short trip that turned out to be a pricey one. Weeks later Chan got a bill for $2,255 from Royal Ambulance, the company that provided her ride. Documents show their insurance paid $573.91, but it appeared the Chan's were on the hook for the rest.
"I was so shocked," Chan said. "Was this really necessary?"
The Chans told the I-Team they were stuck sorting this out for five days as both El Camino Health and Royal Ambulance pointed fingers at each other. According to Chan, a manager at Royal Ambulance told him on the phone: "Yes, this is your bill. You have to pay for it."
Then Chan said he called the ER desk at El Camino Health only to be transferred to a manager who didn't call him back.
Stephanie Sierra: "You called El Camino hospital how many times to sort this out over the past five days?"
Frank Chan: "13 times."
MORE: Medical debt dropped from credit scores: Here's how you can make sure it's removed
The ABC7 News I-Team reached out to El Camino Health and Royal Ambulance, but both agencies were unavailable for an on-camera interview. In an email, El Camino Health told the I-Team:
"If a patient arrives in our emergency room and it is determined they need care that is required in a building not connected to the hospital, professional medical transport is required to ensure patient safety. El Camino Health funds this service and the patient should never receive a bill. We have since been in contact with Royal Ambulance and they have rectified this matter."
The I-Team received this statement during the interview with Chan.
Stephanie Sierra: "Did you get confirmation from El Camino Hospital that they will cover the rest of that payment?"
Frank Chan: "No confirmation yet...even this morning they are still pointing me to Royal Ambulance."
Royal Ambulance told the I-Team, Chan's insurance plan underpaid the claim. The company says they offered to help have the claim reprocessed to reduce expenses, but ultimately waived the unpaid portion as a courtesy-prior to any contact with ABC7.
MORE: Uninsured and Unprotected: Data shows growing health insurance gap across the Bay Area
In the end, the bill sent to Chan was a mistake. But, by the time El Camino Health reported that to the I-Team, Chan said he still had no idea.
"I was not made aware the bill was cleared until ABC7 contacted them," he told the I-Team.
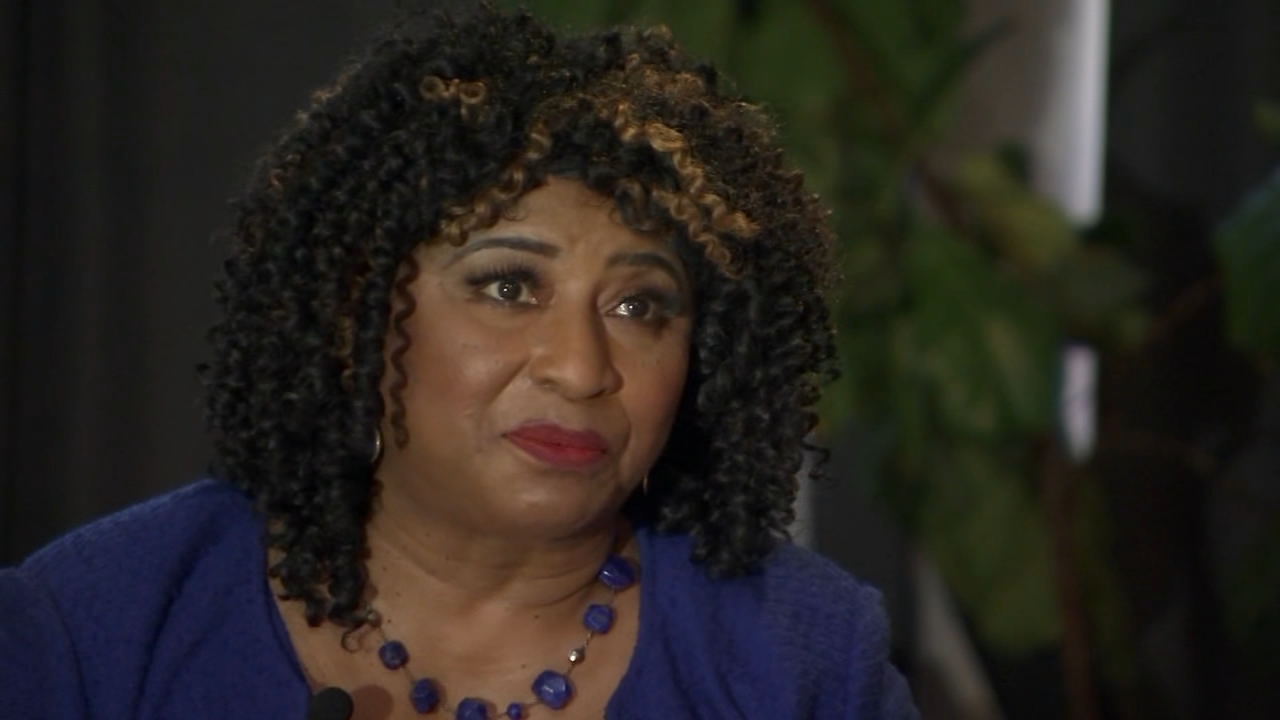
"It should not take hours on the phone or the intervention of a news station to get a hospital to correct their billing," said Carmen Balber, the executive director of Consumer Watchdog.
Stephanie Sierra: "How often do you see cases like this where consumers get overcharged or get a bill that's wrong?"
Carmen Balber: "It happens all the time... patients are charged for procedures that never happen, patients are billed for doctors they never saw, patients are billed for charges that they legally are not required to pay."
As Balber explains, it takes looking at the bill and not just paying by reflex to find those discrepancies. If this happens to you, get a full accounting from the hospital and request that they itemize what each charge is for. State law requires hospitals to let patients know if they qualify for financial assistance.
VIDEO: How to figure out complicated medical bills

"But, all too frequently that's a page and a form the patient misses when they're in the middle of an emergent medical situation," Balber said. "Then they end up with a huge bill on the back end."
Charged upfront -- forced to ask questions later.
This brings us back to Chan's case. While his wife wasn't eligible for financial assistance, they still ended up with a big bill.
"I think it's very unfair," said Chan. "The process was frustrating."
But, thankfully one hour after Chan's interview with the I-team, he said he finally got some answers.
"It was from Royal Ambulance," Chan said. "They said the bill has been cleared and I don't owe them anything... thank you so much."
Another tip for consumers - hospitals may bill for what's called 'out-of-network' charges which are often expensive, but can be challenged. Remember, always read the fineprint and don't pay for a bill in question until the agency can explain the charge.
If you're on the ABC7 News app, click here to watch live